In the case of breast cancer, the aim of surgery is to remove the tumour and analyse the lymph nodes in the armpit (lymphadenectomy), always with the premise of opting for the least aggressive surgical technique adapted to the individual. Basically, there are two main types of surgery for women with breast cancer:
- Breast-conserving surgery and mastectomy. Breast-conserving surgery is the least aggressive technique, as a partial removal of the breast is performed and the breast is not completely resected, unlike a mastectomy. The tumour is removed, with safe surgical margins and then local or loco-regional radiotherapy is administered to eliminate any tumour cells that may remain after the surgery.
- Mastectomy. In this type of surgery, the entire breast is removed, which may or may not include the nipple-areola complex. During the same surgery, it is possible to reconstruct the breast (immediate reconstruction), or it can be done once the complementary treatments have been completed (deferred reconstruction).
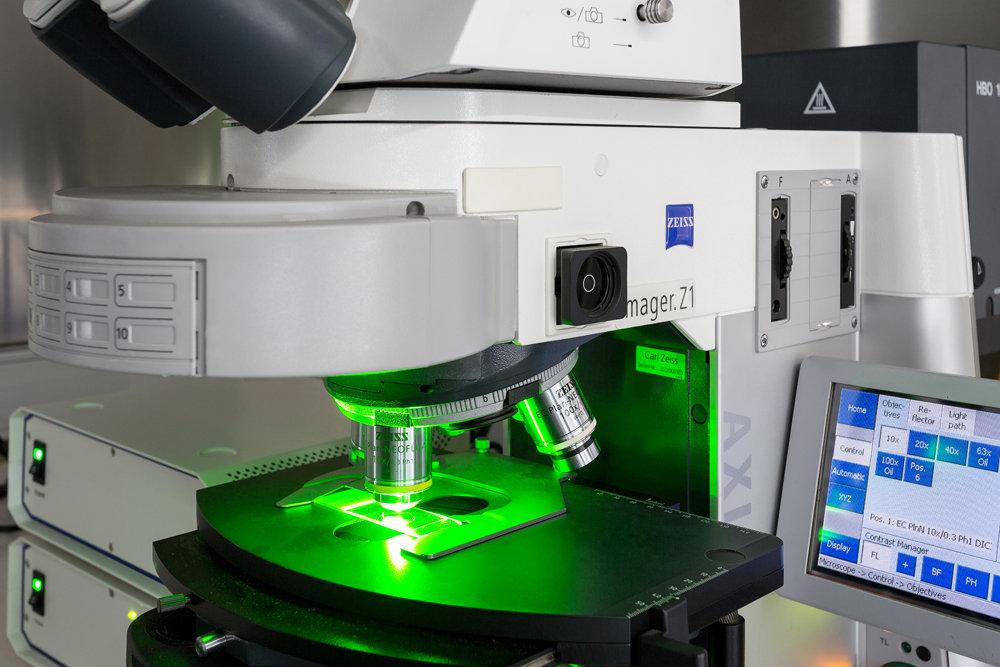
One of the first sites where breast cancer spreads is to the lymph nodes in the armpit. The extent to which this occurs will determine the prognosis of the breast cancer. The only way to know if breast cancer has spread to these lymph nodes in the armpit is to examine them under the microscope. To do this, some nodes have to be removed and then analysed. This procedure has side effects that can be very uncomfortable, such as temporary limitation of arm movement and numbness or swelling of the arm (also known as lymphoedema).
In a specific group of patients, especially those in whom there is clinically no tumour involvement of the sentinel nodes, an alternative to lymphadenectomy may be sentinel lymph node biopsy. The sentinel node is the first node where the tumour is likely to spread. The procedure involves injecting a radioactive substance near the tumour that will flow through the lymphatic ducts to the lymph nodes, detecting which lymph node is the first to receive the substance and testing it after removal. If the result is negative, the lymphadenectomy is no longer necessary and the patient can avoid the side effects described above.
Radiation therapy is a type of treatment that uses ionising radiation to destroy tumour cells and prevent their growth. It damages the DNA of these cells, causing them to die. It is used as a complementary treatment to surgery. It is usually performed after conservative surgery or, in some cases, after a mastectomy.
Radiation therapy can be performed on the breast, chest wall and/or loco-regional lymph node areas such as the axilla or supraclavicular level. The usual form of administration is external radiation therapy, administered by means of a machine (linear accelerator). The duration of treatment can vary from days to weeks, depending on different factors, and just like with surgery, effective strategies with the shortest possible duration and with the least possible associated side effects will always be sought out.
As a complementary treatment to external radiation therapy or as an alternative in some cases, internal radiotherapy or brachytherapy is also used, which consists of injecting radioactive material into the area of the tumour.
Chemotherapy is the administration of drugs, usually intravenously, with the aim of destroying tumour cells scattered throughout the body that surgery and radiation therapy cannot attack. It is described as an adjuvant treatment when administered after surgery, whereas it is called neoadjuvant chemotherapy if chemotherapy is used to shrink the tumour before surgery. The decision to administer the treatment before or after surgery will be made by the multidisciplinary committee and then agreed upon with the patient’s consent.
Chemotherapy treatment is administered in cycles, and the duration and number of cycles will depend on each case. Each cycle lasts on average between once a week or every 2-4 weeks, and the reason why a chemotherapy treatment is administered in cycles is due to the effectiveness of the treatment itself: the treatment is administered in cycles in order to attack the cancer cells when they are most vulnerable and to give the body’s healthy, normal cells time to recover from the damage suffered by the treatment.
Chemotherapy usually causes a series of side effects, including fatigue, nausea and vomiting and temporary hair loss, among others. As with local therapies (surgery and radiotherapy), chemotherapy is intended to be administered only to those patients where the potential benefits, in terms of reducing the risk of recurrence, outweigh the side effects. The current use of genomic platforms can reduce the administration of chemotherapy in up to 40% of cases. In our centre, it is possible to request this determination in those cases in which it is indicated.
Oestrogen and progesterone are sex hormones that are naturally present in women. As previously discussed, some breast tumours depend on the supply of these two substances to grow, and as many as 70% of breast cancers do. When tumour cells retain these hormone receptors, it is possible to administer a drug or hormone treatment that has been shown to reduce the risk of tumour relapse and improve survival rates. Hormone therapy can be administered orally and has fewer side effects than other treatments, such as chemotherapy. The duration of this treatment may range from 5 to 10 years. Monitoring of possible side effects is carried out by the medical oncologist, so the patient will attend quarterly or semi-annual check-ups to find out about possible side effects, as well as any symptoms related to other treatments or those that could lead to the suspicion of a possible tumour recurrence.
Between 15-20% of breast cancers present with an overexpression of the HER2 protein, and these are known as HER2-positive tumours. HER2 proteins are found on the surface of breast cells. HER2 is a transmembrane protein, which spans the entirety of the cell membrane and is involved in normal cell growth. When the tumour has a high amount of this protein, the cancer tends to spread faster than other types of breast cancer. There are now drugs known as monoclonal antibodies (trastuzumab and pertuzumab), which act on tumour cells that can overproduce the HER2 protein, stopping or reducing their growth. In other words, these drugs have the potential to change the nature of this subtype of breast cancer and turn a poor prognosis to a good prognosis due to their high efficacy. These agents are usually administered in combination with chemotherapy for twelve months.